Navigating the complexities of healthcare billing can feel overwhelming, especially when it comes to understanding HCPCS modifiers. These essential codes play a crucial role in ensuring accurate reimbursement and compliance with regulations. But do you know how they can impact your practice’s revenue cycle?
Overview of HCPCS Modifiers
HCPCS modifiers play a vital role in healthcare billing, influencing reimbursement accuracy and compliance. These two-character codes provide additional information about the service or procedure performed.
Definition of HCPCS Modifiers
HCPCS modifiers are alphanumeric codes used to clarify services rendered. For instance, you might encounter modifier -25, indicating that a significant, separately identifiable evaluation and management service occurred on the same day as another procedure. This specificity ensures proper reimbursement for services.
Importance of HCPCS Modifiers
HCPCS modifiers enhance clarity in medical billing processes. They help differentiate between similar services to reflect true clinical scenarios. By using these modifiers accurately, you can:
- Improve claim approval rates.
- Reduce denials related to insufficient documentation.
- Ensure compliance with payer regulations.
Using modifiers correctly contributes directly to your practice’s revenue cycle by minimizing payment delays and maximizing reimbursements for the care provided.
Categories of HCPCS Modifiers
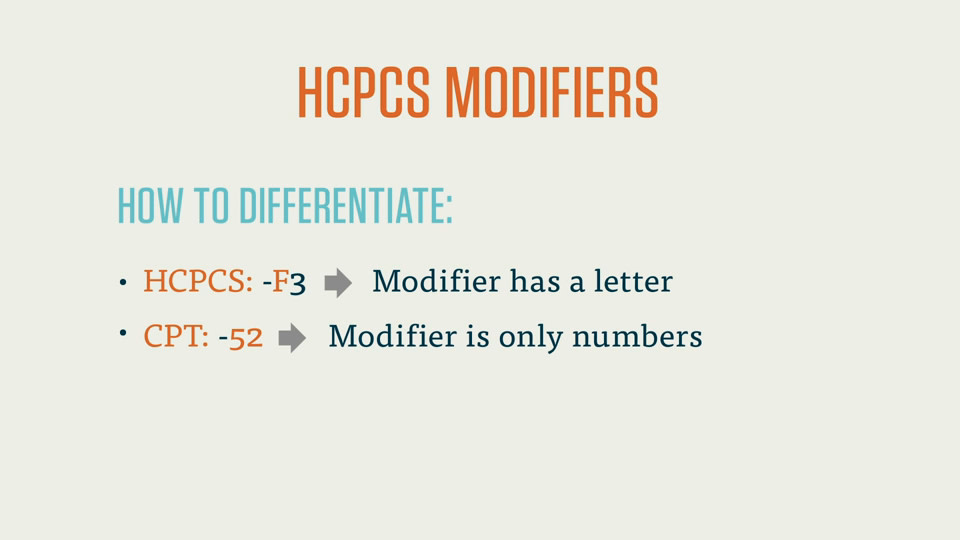
HCPCS modifiers fall into two main categories: Level I and Level II modifiers. Each category serves distinct purposes in medical billing, providing crucial details that enhance the accuracy of claims.
Level I Modifiers
Level I modifiers consist of two-digit numeric codes. They primarily serve to indicate variations in services provided. Common examples include:
- Modifier -25: Indicates a significant, separately identifiable evaluation and management service performed on the same day as another procedure.
- Modifier -50: Used to denote bilateral procedures performed during the same session.
- Modifier -59: Indicates distinct procedural services that are not normally reported together.
These codes help clarify specific situations, ensuring proper reimbursement and compliance with regulations.
Level II Modifiers
Level II modifiers comprise alphanumeric codes and provide additional context for services or equipment. Examples include:
- Modifier KX: Indicates that specific criteria have been met for coverage requirements.
- Modifier GA: Used when a waiver of liability statement is on file for non-covered services.
- Modifier GY: Signifies that a service is statutorily excluded from Medicare coverage.
By utilizing these modifiers effectively, you can improve claim accuracy and reduce denial rates, ultimately benefiting your practice’s revenue cycle.
Commonly Used HCPCS Modifiers
HCPCS modifiers play a critical role in healthcare billing, providing necessary information that impacts reimbursement. Below are some commonly used modifiers and their specific applications.
Examples of Common Modifiers
- Modifier -25: Indicates a significant, separately identifiable evaluation and management service performed on the same day as another procedure.
- Modifier -50: Used for bilateral procedures to signify that the same procedure was performed on both sides of the body.
- Modifier -59: Denotes distinct procedural services when multiple procedures are performed but not related to one another.
- Modifier KX: Shows that specific coverage criteria have been met for certain services or items.
- Modifier GA: Indicates that a waiver of liability has been signed by the patient, acknowledging potential non-payment by Medicare.
- Modifier GY: Applied when a service is excluded from Medicare coverage.
- Modifier -25
- You can use this modifier when an office visit occurs alongside another procedure. For example, if you perform a minor surgical procedure and also conduct an evaluation during the same appointment, attach modifier -25 to clarify that both services were necessary.
- Modifier -50
- This modifier applies when performing surgery on both sides of the body. Suppose you perform knee arthroscopy on each knee; using modifier -50 ensures proper reimbursement for both procedures without confusion.
- Modifier -59
- When delivering unrelated or distinct services in one session, it’s crucial to apply this modifier. If you conduct two different diagnostic tests back-to-back, using modifier -59 shows they’re separate actions deserving full payment.
- Modifier KX
- For durable medical equipment (DME), this modifier confirms compliance with payer requirements. If your practice dispenses specialized wheelchairs meeting Medicare criteria, include KX to validate coverage eligibility.
- Modifier GA
- Using this indicates you’ve informed patients about potential out-of-pocket costs due to non-covered services under Medicare guidelines. It protects your practice from unexpected denials while ensuring transparency with patients.
- Modifier GY
- Apply this when offering non-covered services under Medicare plans. If you’re providing cosmetic surgery or other elective treatments typically excluded from coverage, attaching GY clarifies these limitations upfront.
Understanding these examples helps streamline your billing process and enhances communication with payers regarding claims submissions and reimbursements effectively.
Impact of HCPCS Modifiers on Billing
HCPCS modifiers significantly influence billing practices, impacting reimbursement accuracy and overall revenue. By providing essential details about services rendered, these modifiers help clarify the nature of claims submitted to payers.
How Modifiers Affect Reimbursements
Modifiers directly affect reimbursements by enhancing specificity in claims. For example, modifier -25 indicates that a significant evaluation and management service occurred alongside another procedure. This modifier allows you to receive appropriate payment for both services instead of just one. Similarly, modifier -50 signals bilateral procedures, ensuring proper compensation for treatments involving both sides of the body.
Moreover, using modifier -59 identifies distinct procedural services when multiple unrelated procedures are performed during the same session. This distinction can lead to increased reimbursement opportunities by preventing denials based on perceived overlap in services provided.
Best Practices for Using Modifiers
Utilizing HCPCS modifiers effectively requires attention to detail and adherence to best practices:
- Review documentation: Ensure all relevant documentation supports the use of specific modifiers.
- Stay updated: Regularly check for changes in payer policies regarding modifier usage.
- Educate staff: Train your billing team on correct modifier application to minimize errors.
- Use modifiers judiciously: Apply only when necessary; overusing them may trigger audits or scrutiny from payers.
Incorporating these best practices into your billing process enhances compliance and maximizes reimbursement potential while reducing denial rates associated with incorrect modifier usage.
Future Trends in HCPCS Modifiers
As the healthcare landscape evolves, HCPCS modifiers will continue to play a critical role in billing practices. Staying informed about future trends can enhance your billing accuracy and compliance.
Changes in Regulations
Regulatory updates often prompt changes in how HCPCS modifiers are utilized. For instance, recent modifications might include:
- New coding guidelines that clarify modifier usage
- Updates to existing modifiers based on payer feedback
- Increased scrutiny on specific modifiers leading to stricter enforcement
These changes require you to keep abreast of regulatory shifts. Failing to adapt could lead to claim denials or delayed reimbursements.
Technology’s Role in Modifier Utilization
Technology significantly impacts how you apply HCPCS modifiers. Advanced billing software now offers features like:
- Automated modifier suggestions, reducing manual errors
- Real-time claims tracking, allowing for immediate adjustments
- Data analytics tools that provide insights into modifier performance
Embracing these technologies enhances efficiency and accuracy. Moreover, it streamlines communication with payers, making the claims process smoother overall.