Ever wondered why some bacteria are classified as gram positive while others are gram negative? Understanding this distinction is crucial in microbiology and medicine. Gram positive and gram negative bacteria examples play a significant role in health, disease, and even the food industry.
Overview of Gram Positive and Gram Negative Bacteria
Gram positive and gram negative bacteria play crucial roles in microbiology. Understanding their characteristics helps in identifying their impacts on health, disease, and food safety.
Definition of Gram Staining
Gram staining is a laboratory technique that classifies bacteria based on their cell wall structure. It involves applying crystal violet dye followed by iodine, which forms a complex within the cell walls. After washing with alcohol or acetone, gram positive bacteria retain the dye due to their thick peptidoglycan layer, appearing purple under a microscope. In contrast, gram negative bacteria lose the dye and take up safranin counterstain instead, appearing pink.
Importance of Classification
Classifying bacteria as gram positive or gram negative matters for several reasons:
- Treatment Decisions: Different types respond to antibiotics differently.
- Pathogenicity: Some strains cause serious infections; knowing the type aids diagnosis.
- Food Safety: Certain species are harmful; classification helps prevent contamination.
By distinguishing between these two groups, you gain insights into bacterial behavior and treatment options.
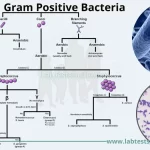
Characteristics of Gram Positive Bacteria
Gram positive bacteria display unique characteristics that set them apart from their gram negative counterparts. They possess a thick peptidoglycan layer in their cell wall, allowing them to retain the crystal violet dye during the gram staining process. This results in a purple appearance under a microscope. Their simpler cell structure contributes to specific responses to antibiotics and immune system attacks.
Structural Features
Gram positive bacteria have several notable structural features:
- Thick Peptidoglycan Layer: This layer provides rigidity and strength, making these bacteria more resistant to certain environmental stresses.
- Teichoic Acids: Present in the cell wall, these acids play roles in maintaining cell shape and regulating ion movement.
- Absence of Outer Membrane: Unlike gram negative bacteria, they lack an outer membrane, which influences their susceptibility to antibiotics.
- Cytoplasmic Membrane: Located beneath the peptidoglycan layer, it contains proteins that facilitate nutrient transport.
These structural elements contribute significantly to how gram positive bacteria interact with their environments.
Common Examples
Some common examples of gram positive bacteria include:
- Staphylococcus aureus: Known for causing skin infections and food poisoning.
- Streptococcus pneumoniae: A leading cause of bacterial pneumonia and meningitis.
- Bacillus anthracis: The bacterium responsible for anthrax infections.
- Clostridium tetani: Causes tetanus through its neurotoxin production.
Characteristics of Gram Negative Bacteria
Gram negative bacteria possess distinct features that set them apart from their gram positive counterparts. Their cell walls have a thin peptidoglycan layer, which doesn’t retain the crystal violet stain during gram staining, leading to a pink appearance. Additionally, they feature an outer membrane containing lipopolysaccharides, contributing to their virulence and resistance to certain antibiotics.
Structural Features
- Thin Peptidoglycan Layer: This layer is significantly thinner than that found in gram positive bacteria, affecting how these organisms react to antibiotics.
- Outer Membrane: The presence of this membrane provides an extra barrier against environmental factors and antimicrobial agents.
- Lipopolysaccharides (LPS): These molecules are crucial for immune system interaction and can trigger strong inflammatory responses in hosts.
Common Examples
Several important examples highlight the relevance of gram negative bacteria:
- Escherichia coli (E. coli): Often found in the intestines, some strains cause foodborne illness.
- Salmonella spp.: This genus includes pathogens responsible for salmonellosis, commonly linked to contaminated food.
- Pseudomonas aeruginosa: Known for its resistance to antibiotics, it poses risks in hospital settings, especially for immunocompromised patients.
- Neisseria meningitidis: A significant cause of bacterial meningitis, this organism requires prompt treatment to reduce mortality.
Understanding these characteristics aids in identifying and addressing infections caused by gram negative bacteria effectively.
Differences Between Gram Positive and Gram Negative Bacteria
Understanding the differences between gram positive and gram negative bacteria is crucial for microbiology, health, and food safety. Key distinctions lie in their cell wall composition and antibiotic responses.
Cell Wall Composition
Gram positive bacteria feature a thick peptidoglycan layer, which retains the crystal violet stain during gram staining, giving them a purple appearance. Their cell walls also contain teichoic acids, contributing to structural integrity. Examples of gram positive bacteria include:
- Staphylococcus aureus: Known for causing skin infections.
- Streptococcus pneumoniae: Associated with pneumonia.
- Bacillus anthracis: The causative agent of anthrax.
- Clostridium tetani: Responsible for tetanus.
In contrast, gram negative bacteria have a thin peptidoglycan layer surrounded by an outer membrane rich in lipopolysaccharides. This structure prevents retention of the crystal violet stain, resulting in a pink appearance. Common examples include:
- Escherichia coli (E. coli): Linked to foodborne illnesses.
- Salmonella spp.: Often associated with gastrointestinal infections.
- Pseudomonas aeruginosa: Known for its resistance to antibiotics.
- Neisseria meningitidis: A cause of bacterial meningitis.
Response to Antibiotics
Gram positive bacteria are typically more susceptible to antibiotics that target peptidoglycan synthesis due to their thick cell walls. For instance, penicillin effectively disrupts their cell wall formation.
On the flip side, gram negative bacteria exhibit greater resistance because of their outer membrane that acts as a barrier against many antibiotics. They often require different treatment strategies using drugs like aminoglycosides or fluoroquinolones.
Recognizing these differences aids in making informed decisions about treatment options and understanding pathogenicity in various contexts.