Imagine a healthcare system where every aspect of your well-being is seamlessly connected. This is the promise of a full continuum of care, ensuring that you receive comprehensive support at every stage of your health journey. From prevention and acute treatment to rehabilitation and ongoing management, this approach focuses on delivering personalized care tailored to your needs.
In this article, you’ll discover real-world examples of how the full continuum of care transforms lives. Have you ever wondered how coordinated services can enhance recovery or improve quality of life? By exploring various models and success stories, you’ll gain insights into the benefits and challenges associated with implementing such an integrated system. Get ready to delve deeper into a healthcare strategy that prioritizes continuity, efficiency, and above all, your health.
Understanding Full Continuum of Care
The full continuum of care encompasses a range of services designed to support individuals throughout their health journey. This approach ensures that care is available at various stages, addressing prevention, treatment, and ongoing management needs.
Definition and Scope
The full continuum of care refers to an integrated system offering comprehensive healthcare services. It includes several key components:
- Preventive Services: Regular screenings and vaccinations aim to identify potential health issues early.
- Acute Care: Immediate medical attention for serious conditions or emergencies.
- Chronic Disease Management: Ongoing support for individuals with long-term health issues such as diabetes or heart disease.
- Rehabilitation Services: Physical therapy and counseling assist in recovery after illness or injury.
- Palliative Care: Specialized care focused on providing relief from symptoms and improving quality of life for patients with serious illnesses.
By covering these areas, the full continuum addresses all aspects of an individual’s healthcare needs.
Importance in Healthcare
Implementing a full continuum of care leads to numerous benefits in the healthcare system. For instance:
- Improved Patient Outcomes: Coordinated services enhance recovery rates by ensuring seamless transitions between different levels of care.
- Cost Efficiency: Preventive measures reduce the need for more expensive treatments down the line.
- Patient Satisfaction: Personalized experiences foster trust between patients and providers, leading to better adherence to treatment plans.
You might wonder how this model affects your personal healthcare experience. When you encounter integrated systems, you receive tailored support that aligns with your unique needs, promoting overall wellness effectively.
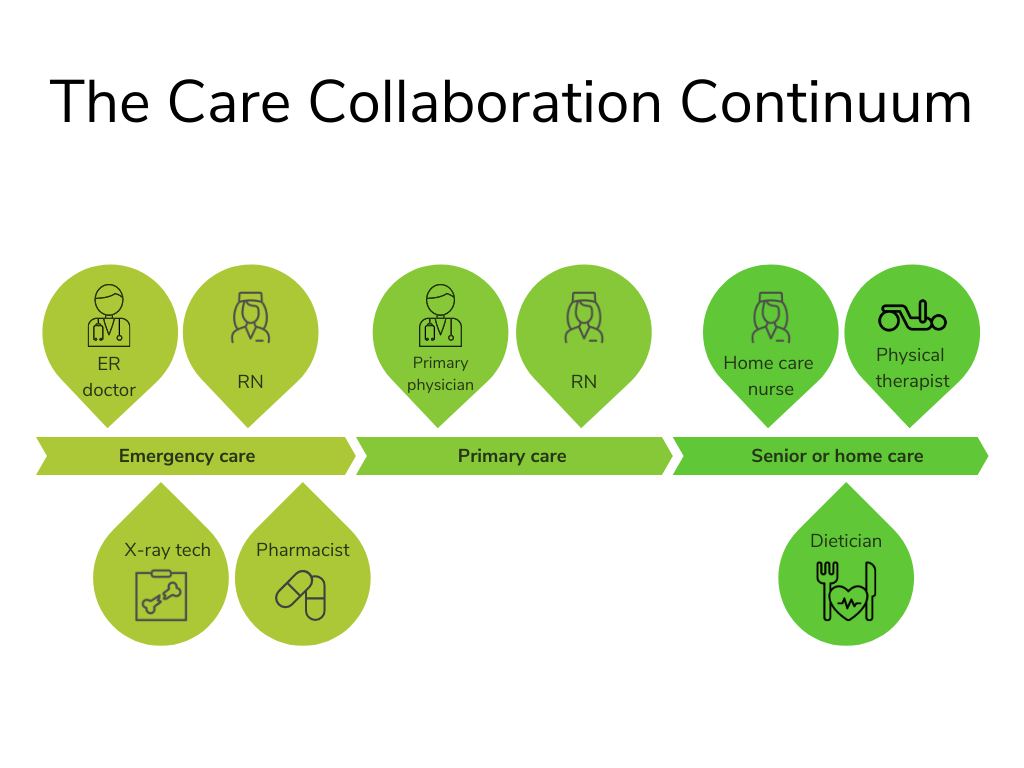
Components of Full Continuum of Care
The full continuum of care incorporates various essential components that work together to support individual health needs throughout their journey. Understanding these components enhances the overall effectiveness of healthcare delivery.
Primary Care
Primary care serves as the foundation for the full continuum. It involves regular check-ups, preventive screenings, and management of chronic conditions. Strong relationships with primary care providers lead to better patient outcomes by ensuring continuity in treatment plans. For example, a patient with diabetes benefits from ongoing monitoring and education about lifestyle changes. This proactive approach helps prevent complications and promotes overall well-being.
Specialized Services
Specialized services address specific health issues that require expert attention. These services include cardiology, oncology, and mental health support. Access to specialized care ensures patients receive tailored treatments based on their unique conditions. For instance, an individual diagnosed with cancer may need chemotherapy or radiation therapy alongside psychological counseling. Coordinated efforts between specialists enhance recovery rates and improve quality of life.
Post-Acute Care
Post-acute care focuses on rehabilitation and recovery after hospital stays or surgeries. This component includes home health services, skilled nursing facilities, and outpatient therapy programs. Effective post-acute care reduces readmission rates by providing continued support during recovery stages. A patient recovering from knee surgery might utilize physical therapy sessions at home while receiving follow-up visits from a nurse for wound management.
These components collectively create a robust framework for delivering comprehensive healthcare tailored to your needs at every stage of your health journey.
Benefits of Full Continuum of Care
A full continuum of care offers numerous advantages that significantly enhance the healthcare experience. This model ensures individuals receive tailored support throughout their health journey, leading to better outcomes and overall satisfaction.
Improved Patient Outcomes
Improved patient outcomes are a significant benefit of the full continuum of care. When patients access coordinated services like preventive care, acute treatment, and ongoing management, they experience better overall health. For example:
- Chronic Disease Management: Regular monitoring and personalized plans lead to fewer hospital admissions for conditions like diabetes or heart disease.
- Follow-Up Care: Patients receiving follow-up appointments after surgeries or treatments often report quicker recoveries.
Additionally, this approach fosters strong relationships between patients and healthcare providers. Such relationships create trust, making patients more likely to adhere to treatment plans.
Cost-Effectiveness
Cost-effectiveness is another key advantage of implementing a full continuum of care. By addressing health issues early through preventive measures, healthcare systems can reduce expensive emergency interventions. Consider these points:
- Reduced Hospital Readmissions: Comprehensive post-discharge support decreases the likelihood of readmission within 30 days.
- Lower Overall Healthcare Costs: Continuous care reduces duplication in services and tests, saving money for both patients and providers.
Moreover, investing in preventative services pays off by improving long-term health outcomes while minimizing expenses associated with chronic illnesses.
Challenges in Implementing Full Continuum of Care
Implementing a full continuum of care faces several challenges that can hinder its effectiveness. Understanding these obstacles is crucial for developing strategies to overcome them.
Coordination of Services
Effective coordination among various healthcare providers remains a significant challenge. Many systems operate independently, leading to fragmented care. For instance, if a patient receives treatment from multiple specialists without proper communication, it may result in conflicting advice or duplicate tests. Additionally, inconsistent electronic health records can complicate information sharing between facilities. Establishing standardized protocols and integrated platforms can help streamline this process.
Funding and Resources
Insufficient funding often limits the availability of essential services. Many healthcare organizations struggle to allocate resources effectively across all areas needed for a full continuum of care. When budgets are tight, preventive services may take precedence over chronic disease management programs. Consequently, this can lead to increased hospital readmissions and higher overall costs. Advocating for policy changes that prioritize comprehensive funding models is necessary for sustainable implementation.