Imagine a world where nurses make critical decisions independently, shaping patient care with their expertise. Examples of autonomy in nursing highlight the profound impact these professionals have on healthcare outcomes. Autonomy empowers nurses to assess situations, prioritize tasks, and implement interventions without waiting for directives from physicians.
In this article, you’ll discover real-life instances where nurses exercise their judgment and skills to enhance patient well-being. From managing medication regimens to advocating for patients’ needs, each example illustrates how autonomy not only benefits individuals but also elevates the entire healthcare system. Are you ready to explore the dynamic role of autonomy in nursing? Dive in and see how these empowered professionals redefine patient care every day.
Importance of Autonomy in Nursing
Autonomy in nursing plays a critical role in enhancing patient care. Nurses who exercise their autonomy can respond swiftly to patients’ needs, ensuring timely interventions. This ability leads to improved healthcare outcomes and higher patient satisfaction.
Consider these examples where autonomy significantly impacts nursing practice:
- Medication Management: Nurses independently assess medication effectiveness and adjust dosages based on patient responses.
- Patient Advocacy: Nurses advocate for patients’ rights and preferences, often making decisions that align with individual values.
- Care Planning: Nurses develop personalized care plans by evaluating diverse factors like medical history and current health status.
These instances illustrate how autonomy empowers nurses to make informed decisions that directly affect treatment quality. By trusting their judgment, healthcare systems benefit from enhanced efficiency and reduced errors.
Examples of Autonomy in Nursing Practice
Autonomy in nursing manifests through various practices, allowing nurses to make independent decisions that directly affect patient care. Here are specific examples illustrating this vital aspect.
Patient Care Decisions
Nurses frequently exercise autonomy in making patient care decisions. For instance, they assess patients’ conditions and determine necessary interventions, such as:
- Adjusting medication dosages based on patient responses.
- Implementing emergency protocols when sudden health changes occur.
- Educating patients about their health conditions and treatment options.
Such actions demonstrate how nurses prioritize individual needs and ensure tailored care.
Personal Nursing Philosophy
A strong personal nursing philosophy allows you to advocate for diverse patient needs effectively. Many nurses develop unique approaches that guide their practice, including:
- Holistic assessments, considering physical, emotional, and social factors.
- Patient-centered communication, fostering trust and openness.
- Ethical decision-making, balancing professional standards with compassion.
By adhering to these principles, you enhance the quality of care while respecting each patient’s individuality.
Leadership Roles
Nurses often step into leadership roles that require autonomous decision-making. In these positions, they might:
- Lead interdisciplinary teams during patient rounds.
- Develop clinical protocols based on evidence-based practices.
- Mentor newer staff members, sharing knowledge and promoting best practices.
These responsibilities not only shape healthcare delivery but also empower other professionals within the team to strive for excellence.
Benefits of Autonomy in Nursing
Autonomy in nursing brings several advantages that enhance both patient care and the work environment for nurses. These benefits highlight why empowering nurses to make independent decisions is crucial.
Improved Patient Outcomes
Autonomous decision-making leads to better patient outcomes. When nurses assess patients independently, they can implement timely interventions. For example:
- Medication adjustments: Nurses can modify dosages based on individual responses.
- Emergency protocols: They can act quickly during critical situations, ensuring immediate care.
- Patient education: By providing tailored information, nurses empower patients to manage their health effectively.
Such actions contribute to a more responsive healthcare system, ultimately improving recovery rates and reducing complications.
Enhanced Job Satisfaction
Nursing autonomy significantly boosts job satisfaction. When you have the freedom to make clinical decisions, it fosters a sense of ownership over your practice. Consider these factors:
- Increased confidence: You develop stronger skills through independent practice.
- Greater professional respect: Autonomy cultivates recognition from peers and other healthcare professionals.
- Better work-life balance: Empowered nurses often experience less burnout due to their ability to prioritize tasks effectively.
These aspects create a fulfilling work environment that attracts and retains skilled nursing talent.
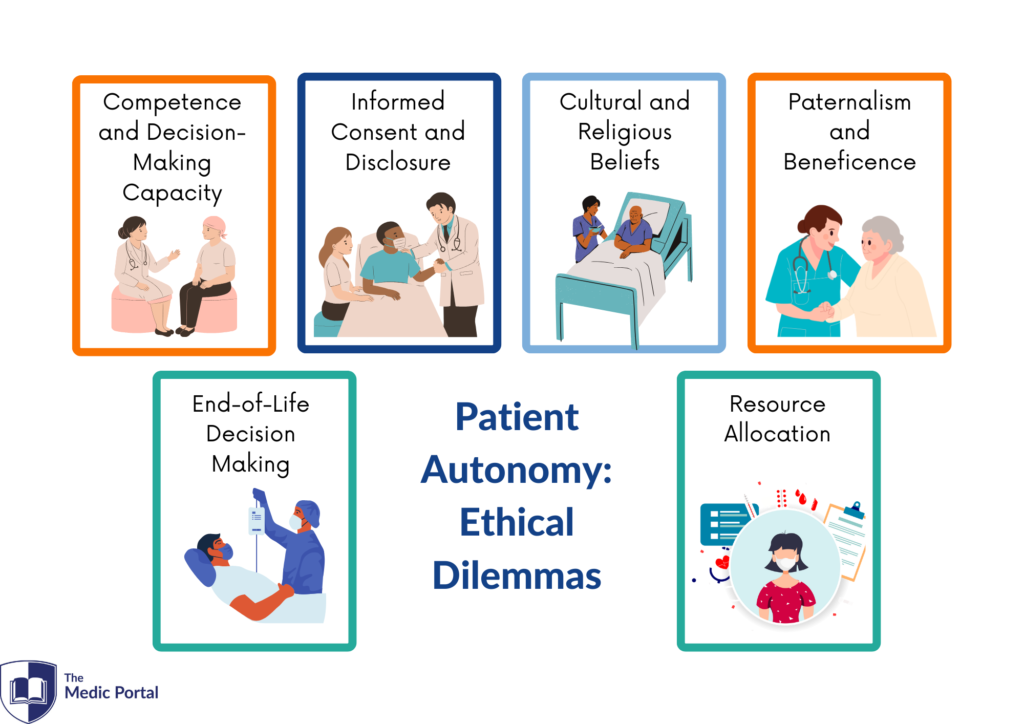
Challenges to Autonomy in Nursing
Autonomy in nursing faces several significant challenges that can hinder effective patient care. Understanding these obstacles is crucial for fostering an environment that supports nurses’ independent decision-making.
Institutional Barriers
Institutional barriers often limit nurses’ autonomy. For example,
- Rigid protocols may restrict a nurse’s ability to use their judgment when responding to unique patient needs.
- Inadequate staffing can lead to increased workloads, making it difficult for nurses to exercise their professional discretion effectively.
- Lack of support from management may discourage nurses from taking initiative or advocating for patients.
These factors create an atmosphere where autonomy becomes challenging, impacting both job satisfaction and patient outcomes.
Interprofessional Dynamics
Interprofessional dynamics also play a role in limiting nursing autonomy. While collaboration among healthcare professionals is vital, sometimes the hierarchical structure within teams can overshadow nurses’ voices. Consider these points:
- Dominance of physicians may result in reluctance from nurses to express differing opinions or suggest alternative treatment plans.
- Communication breakdowns between team members can lead to misunderstandings about roles and responsibilities, further marginalizing nursing contributions.
- Resistance to change among healthcare staff can stifle innovative practices that rely on nurse-led initiatives.
These dynamics highlight the need for stronger interdisciplinary communication and respect for each professional’s expertise.