When you step into a healthcare setting, you might not realize the complex web of decisions that professionals face daily. Ethical dilemmas in healthcare often challenge even the most seasoned practitioners, forcing them to weigh moral principles against practical realities. From end-of-life choices to resource allocation, these dilemmas can significantly impact patient care and outcomes.
Have you ever considered what happens when a doctor must choose between saving one life over another? The tension between doing what’s right and what’s necessary creates scenarios that test the very foundation of medical ethics. This article explores various examples of ethical dilemmas in healthcare, shedding light on real-world situations that provoke thought and discussion. By understanding these challenges, you’ll gain insight into the moral complexities that shape patient care today.
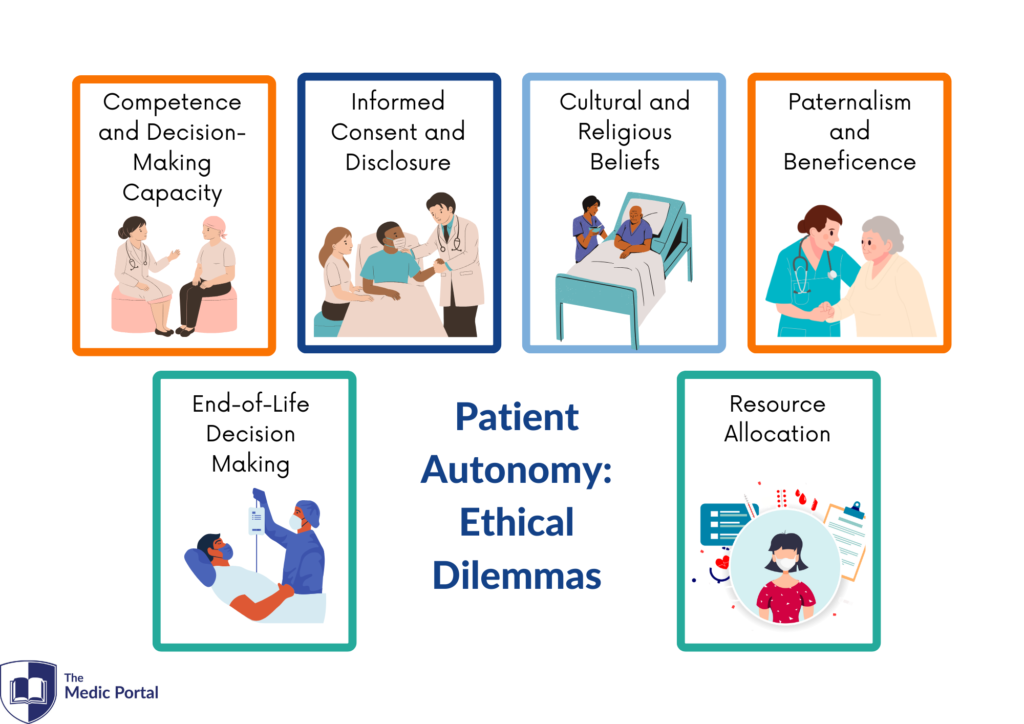
Overview of Ethical Dilemmas in Healthcare
Ethical dilemmas in healthcare frequently arise, challenging professionals to navigate complex situations. One common example involves end-of-life decisions, where patients or families face choices about life-sustaining treatment. These moments test the values of autonomy and beneficence, as healthcare providers strive to respect patient wishes while ensuring quality care.
Resource allocation presents another significant ethical dilemma. Limited medical resources often force tough decisions on who receives treatment. In emergencies or during public health crises, prioritizing patients based on need versus potential outcomes complicates the process further.
Informed consent is also critical. Patients must understand their options before making decisions about procedures or treatments. When a patient lacks capacity due to age or mental state, determining how to proceed can create conflicts between ethical obligations and practical realities.
Healthcare professionals regularly grapple with these examples of ethical dilemmas. Each situation requires careful consideration of moral principles aligned with patient care priorities. As you explore these challenges, reflect on how they shape the future of ethical practices in healthcare settings.
Key Ethical Principles
Healthcare professionals navigate various ethical principles that guide their decision-making processes. Understanding these principles helps clarify the moral dilemmas encountered in practice.
Autonomy
Autonomy emphasizes a patient’s right to make informed decisions about their own healthcare. For instance, when patients refuse treatment, respecting their choice aligns with this principle. This respect fosters trust between patients and providers. Consider a scenario where a patient declines life-sustaining measures; honoring this decision illustrates the application of autonomy even amid emotional turmoil.
Beneficence
Beneficence focuses on actions that promote the well-being of patients. Healthcare providers often strive to provide effective treatments that improve health outcomes. An example includes administering pain relief for terminally ill patients. This proactive approach ensures quality of life during difficult times, reflecting a commitment to beneficence within clinical settings.
Nonmaleficence
Nonmaleficence dictates an obligation not to cause harm to patients. This principle requires careful consideration before proceeding with any intervention. For example, a surgeon must weigh potential risks against benefits before performing surgery. If the procedure poses excessive danger without significant gain, it may be deemed unethical according to nonmaleficence standards.
Justice
Justice refers to fair distribution of healthcare resources and treatment among all individuals. It raises questions about equity in access and availability of services. A pertinent example is prioritizing COVID-19 vaccinations based on vulnerability rather than socioeconomic status. Applying justice ensures that those most in need receive appropriate care, fostering fairness within the healthcare system.
Common Ethical Dilemmas
Ethical dilemmas in healthcare frequently challenge professionals, requiring careful thought and attention. Here are some common examples that illustrate these complexities.
End-of-Life Care
End-of-life care often presents difficult decisions for patients and families. For instance, consider a scenario where a terminally ill patient faces the choice of continuing aggressive treatment or transitioning to palliative care. In such cases, respecting the patient’s wishes while ensuring their comfort becomes vital. Family members might disagree on what’s best, leading to emotional stress and potential conflicts among loved ones.
Informed Consent
Informed consent remains crucial in healthcare settings but can lead to ethical challenges. Imagine a situation where a patient lacks the capacity to understand treatment options due to cognitive impairment. Healthcare providers must navigate this sensitive landscape, balancing the need for consent with the obligation to act in the patient’s best interest. When family members have differing opinions about what constitutes informed consent, it complicates decision-making further.
Resource Allocation
Resource allocation poses significant ethical dilemmas, especially during crises like pandemics. Consider an emergency room overwhelmed with patients needing ventilators; decisions about who receives life-saving equipment become necessary. This scenario raises questions about fairness and equity—should priority go to younger individuals or those with better prognoses? The implications of these choices affect not just individual lives but also broader public health outcomes.
These examples highlight how complex ethical dilemmas shape everyday healthcare decisions, demanding thoughtful consideration from all involved parties.
Case Studies
Ethical dilemmas in healthcare manifest through real-world scenarios that challenge practitioners. Here are some notable examples that illustrate these complexities.
Notable Examples
- End-of-Life Decisions: In one case, a terminally ill patient opted for aggressive treatment despite a poor prognosis. Family members disagreed, believing palliative care offered better quality of life. This situation highlighted the tension between respecting patient autonomy and prioritizing beneficence.
- Informed Consent: A 70-year-old man needed surgery but had cognitive impairments affecting his decision-making capacity. The surgical team faced difficulties when family opinions diverged on whether to proceed with the operation, raising questions about informed consent and ethical obligations.
- Resource Allocation During Crisis: During the COVID-19 pandemic, hospitals experienced ventilator shortages. Healthcare professionals employed triage protocols to prioritize patients based on survival probabilities, emphasizing fairness yet provoking debates over equitable access to life-saving treatments.
- Clinical Trials: An experimental drug showed promise for treating severe illnesses but had significant side effects. Patients faced challenges understanding risks versus benefits as they decided whether to participate in trials, showcasing the importance of clear communication in informed consent processes.
Lessons Learned
From these cases, several key lessons emerge:
- Communication Matters: Clear dialogue among patients, families, and healthcare teams fosters understanding and mitigates misunderstandings.
- Value Autonomy: Respecting patient choices can sometimes lead to conflict; however, recognizing their rights is crucial.
- Prioritize Equity: Fair resource distribution remains vital during crises; transparency in decision-making builds trust within communities.
- Educate Continuously: Ongoing education about ethical principles equips healthcare professionals with tools to navigate complex situations effectively.
These examples serve as reminders of the intricate moral landscape you navigate daily in healthcare settings.