Imagine walking into an emergency room, only to be denied treatment because of your insurance status. This shocking scenario highlights the serious issue of EMTALA violations. The Emergency Medical Treatment and Labor Act was designed to ensure that everyone receives essential medical care regardless of their ability to pay. However, violations occur more often than you might think.
In this article, we’ll explore real-life examples of EMTALA violations and their implications for patients and healthcare providers alike. You’ll discover how these breaches not only affect individual lives but also undermine the integrity of our healthcare system. Are hospitals truly upholding their legal obligations? Join us as we delve into the complexities surrounding EMTALA violations and uncover what they mean for you and your community.
Understanding EMTALA Violations
EMTALA violations occur when hospitals fail to provide adequate emergency medical care regardless of a patient’s ability to pay. These violations can significantly impact patients and their communities.
Definition of EMTALA
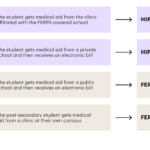
The Emergency Medical Treatment and Labor Act (EMTALA) mandates that hospitals offer emergency services without discrimination. It requires all patients, regardless of insurance status or financial situation, to receive a medical screening examination and necessary treatment for emergencies. Violating this act can lead to serious legal repercussions and penalties for healthcare facilities.
Importance of EMTALA Compliance
EMTALA compliance is vital for protecting patient rights. Ensuring adherence promotes equal access to emergency care, fostering trust in the healthcare system. Non-compliance can result in severe consequences, including fines up to $50,000 per violation and potential lawsuits from affected patients. Hospitals must prioritize compliance not only for legal reasons but also for ethical obligations toward their communities.
Understanding EMTALA violations highlights the necessity of equitable treatment in healthcare settings.
Common Types of EMTALA Violations
EMTALA violations occur in various forms. Understanding these common types can help you recognize the implications for patient care and hospital responsibilities.
Failure to Screen Patients
Failure to provide a medical screening examination constitutes a significant violation. Hospitals must assess all individuals seeking emergency care, regardless of insurance status. For instance, if a patient arrives with chest pain but doesn’t have insurance, the hospital can’t refuse them treatment based solely on their financial situation. Such actions not only compromise patient safety but also violate federal law.
Inappropriate Transfers
Inappropriate transfers of patients between facilities represent another critical violation. Hospitals must ensure that transfers are medically necessary and properly executed. If an unstable patient is moved without adequate justification or consent, this can lead to severe health risks. For example, transferring a stroke patient without stabilizing their condition first poses serious threats to their recovery and well-being. This practice not only violates EMTALA but also endangers lives.
Consequences of EMTALA Violations
EMTALA violations lead to serious repercussions for healthcare providers and patients alike. Understanding these consequences is essential for appreciating the importance of compliance.
Legal Ramifications
Legal penalties for EMTALA violations can be severe. Hospitals face fines up to $50,000 per violation, depending on the severity. The Centers for Medicare & Medicaid Services (CMS) may also impose additional sanctions, such as suspension from Medicare participation. Lawsuits from affected patients can result in costly settlements or judgments against healthcare facilities. For example, a hospital found guilty of failing to screen a patient could face not only financial penalties but reputational damage that affects future business.
Impact on Patient Care
The impact on patient care due to EMTALA violations is profound. When hospitals deny appropriate medical screenings, patients experience delays in critical treatment. Such delays can exacerbate health conditions and lead to avoidable complications or even fatalities. A case study illustrates this risk: A patient seeking emergency care was turned away based on their insurance status; they later suffered a heart attack due to delayed intervention. This highlights how non-compliance compromises safety and undermines trust in the healthcare system.
Case Studies of EMTALA Violations
Examining real-life examples highlights the significant consequences of EMTALA violations. These cases demonstrate how non-compliance affects patients and healthcare providers alike.
Notable Case 1
In a notable case from Texas, a patient arrived at an emergency department with severe chest pain. Instead of receiving immediate medical attention, hospital staff denied treatment based on the patient’s lack of insurance. As a result, the patient experienced a heart attack hours later due to delayed care. This incident underscores that refusing treatment based on insurance status directly violates EMTALA regulations.
Notable Case 2
Another striking example occurred in California when a pregnant woman sought emergency care after experiencing complications. Hospital personnel transferred her to another facility without ensuring proper medical screening or stabilization first. Tragically, the transfer led to complications during labor that could have been prevented with timely intervention. This situation illustrates that inappropriate transfers violate both EMTALA requirements and jeopardize patient safety.
Strategies to Prevent EMTALA Violations
You can implement several strategies to prevent EMTALA violations effectively.
Staff Training and Education
Regular training sessions for staff are crucial. Educate all healthcare personnel on EMTALA requirements, focusing on screening procedures and patient rights. Ensure they understand that every patient deserves a medical screening examination regardless of their insurance status. For example, role-playing scenarios can highlight proper responses in emergencies or situations involving uninsured patients.
Provide ongoing education about legal repercussions. Discuss potential fines or sanctions your facility could face if non-compliance occurs. This knowledge fosters accountability among staff members and emphasizes the importance of adhering to regulations.
Implementation of Protocols
Establish clear protocols for emergency care. Create standard operating procedures that outline steps for conducting medical screenings and transferring patients safely. Ensure these protocols comply with EMTALA guidelines while being easily accessible to all staff members.
Utilize checklists during patient intake. Incorporating a checklist can help ensure no critical steps are overlooked when assessing patients’ needs upon arrival. For instance, include questions regarding insurance status separately from the medical assessment process to avoid bias against uninsured individuals.
Conduct regular audits and assessments. Periodically review compliance with EMTALA regulations through internal audits. Monitoring adherence helps identify areas needing improvement, ensuring continuous quality in emergency care delivery.