Imagine battling not just one but two life-altering conditions at once. Co-occurring disorders can complicate recovery and treatment, making it essential to understand their impact on individuals. These disorders often involve a combination of mental health issues and substance use disorders, creating a challenging landscape for those affected.
In this article, you’ll explore real-life examples of co-occurring disorders that illustrate the struggles many face daily. From anxiety paired with alcohol dependence to depression linked with opioid addiction, these cases highlight the urgent need for integrated treatment approaches. Why is it crucial to address both conditions simultaneously? By shedding light on these intertwined challenges, you’ll gain valuable insights into effective strategies for support and recovery. Join us as we delve deeper into this pressing topic and uncover the complexities surrounding co-occurring disorders.
Understanding Co-Occurring Disorders
Co-occurring disorders involve the simultaneous presence of mental health issues and substance use disorders. This complexity requires a thorough understanding of both conditions for effective treatment.
Definition of Co-Occurring Disorders
Co-occurring disorders refer to the diagnosis of at least one mental health disorder alongside one or more substance use disorders. For instance, someone may experience depression while also struggling with alcohol dependence. Recognizing these overlapping conditions is crucial, as each can exacerbate the other, complicating recovery efforts.
Prevalence and Statistics
Strong statistics illustrate the widespread nature of co-occurring disorders:
- Approximately 7.9 million adults in the U.S. face co-occurring mental health and substance use disorders.
- Studies show that nearly 50% of individuals with severe mental illnesses also have a substance use disorder.
- The National Institute on Drug Abuse reports that around 30% of people with drug abuse problems also experience mental illness.
Causes and Risk Factors
Co-occurring disorders arise from a combination of biological and environmental factors. Understanding these causes contributes to effective treatment strategies.
Biological Factors
Biological factors play a significant role in the development of co-occurring disorders. Genetics can influence both mental health issues and substance use disorders. For example, individuals with a family history of addiction may be more susceptible to developing similar problems themselves. Neurotransmitter imbalances also contribute; conditions like depression or anxiety may lead an individual to self-medicate with substances, creating a cycle that worsens both conditions.
Environmental Influences
Environmental influences significantly impact the likelihood of developing co-occurring disorders. Stressful life events, such as trauma or loss, often trigger mental health issues or substance abuse behaviors. Additionally, exposure to drug use during adolescence can increase vulnerability to addiction later in life. Social factors, including peer pressure and socioeconomic status, also play critical roles in shaping one’s risk for these overlapping conditions.
Impact of Co-Occurring Disorders
Co-occurring disorders significantly affect various aspects of life for individuals and their surrounding environments. Understanding these impacts reveals the urgency for effective treatment and support systems.
On Individuals
Individuals with co-occurring disorders often face heightened challenges in daily functioning. For example, someone battling depression alongside alcohol dependence may struggle to maintain employment due to absenteeism or decreased productivity. Additionally, anxiety coupled with opioid addiction can lead to social withdrawal, making it difficult to form relationships. Studies show that those with both mental health issues and substance use disorders experience more severe symptoms than those dealing with just one condition.
On Families and Communities
<strongFamilies play a crucial role in supporting individuals with co-occurring disorders. Family members might find themselves overwhelmed by the emotional toll of watching a loved one struggle. They often face feelings of helplessness or frustration when trying to encourage treatment adherence. Communities also feel the impact; increased healthcare costs arise from untreated conditions, leading to higher rates of homelessness or crime linked to substance misuse. Support groups within communities can provide vital resources for families navigating these complexities, fostering understanding and resilience among all involved.
Treatment Approaches
Treatment for co-occurring disorders requires a comprehensive strategy that addresses both mental health issues and substance use disorders simultaneously. Focusing on integrated treatment models and evidence-based therapies often leads to better outcomes for individuals facing these challenges.
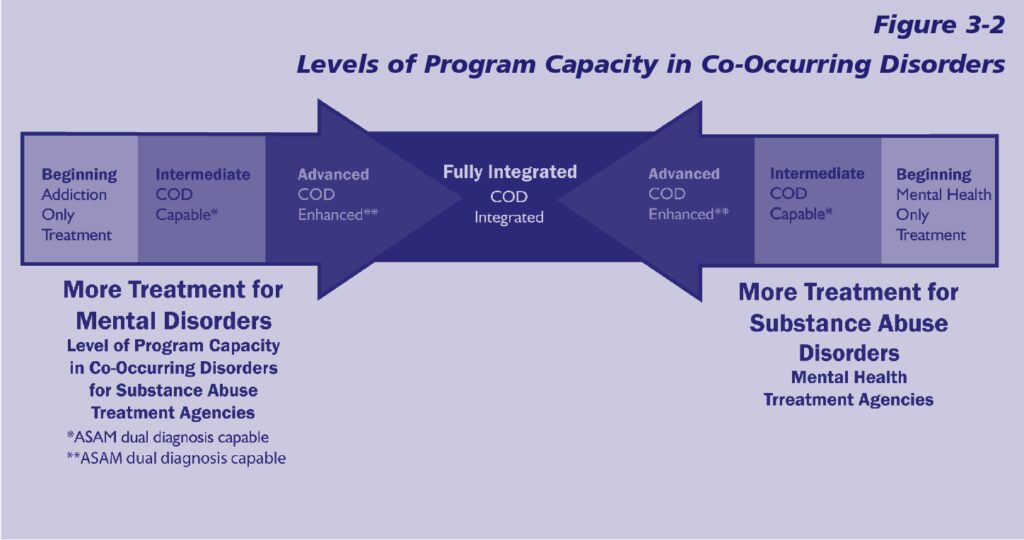
Integrated Treatment Models
Integrated treatment models combine interventions for both mental health and substance use disorders. These approaches recognize the interconnectedness of these conditions, leading to more effective care. For instance:
- Dual Diagnosis Programs: Many facilities offer specialized programs designed specifically for individuals with co-occurring disorders. These programs provide coordinated care from professionals trained in both areas.
- Assertive Community Treatment (ACT): ACT is a team-based approach that delivers comprehensive support in real-world settings, ensuring continuous assistance without overwhelming the individual.
- Case Management Services: Effective case management ensures individuals access needed resources, such as housing, employment support, or therapeutic services tailored to their unique circumstances.
Integrated models facilitate communication among healthcare providers, allowing for consistent monitoring of progress and adjustments to treatment plans as necessary.
Evidence-Based Therapies
Evidence-based therapies play a crucial role in treating co-occurring disorders by utilizing methods proven effective through research. Common evidence-based therapies include:
- Cognitive Behavioral Therapy (CBT): CBT helps individuals identify negative thought patterns and behaviors related to both mental illness and substance abuse. This therapy equips you with coping strategies essential for managing triggers.
- Motivational Interviewing (MI): MI fosters an individual’s motivation to change by exploring ambivalence regarding their substance use while supporting mental wellness goals.
- Dialectical Behavior Therapy (DBT): DBT focuses on emotion regulation skills and interpersonal effectiveness, beneficial for those struggling with mood disorders alongside addiction issues.
These therapies create a supportive framework that encourages long-term recovery by addressing specific needs related to co-occurring disorders effectively.
Challenges in Treatment
Co-occurring disorders present significant challenges in treatment. Individuals face complexities that complicate their recovery journey.
Stigma and Misunderstanding
Stigma surrounding mental health and substance use disorders often prevents individuals from seeking help. Many people fear judgment or alienation, leading to isolation. For instance, someone with anxiety might avoid therapy due to concerns about being seen as weak. Similarly, those battling addiction may refrain from speaking up for fear of being labeled a failure. This stigma can perpetuate the cycle of untreated conditions and worsen overall outcomes.
Accessibility of Services
Accessibility of services remains a critical barrier for many individuals with co-occurring disorders. Limited availability of integrated treatment programs makes it difficult for them to receive proper care. For example:
- Geographic limitations: Rural areas might lack specialized facilities.
- Financial constraints: Insurance coverage may not extend to dual diagnosis treatments.
- Cultural factors: Some communities lack awareness about available resources or view treatment as unnecessary.
These factors hinder access to crucial support systems, leaving many without the help they need for recovery.