Have you ever wondered why some bacterial infections are harder to treat than others? One major factor is the presence of beta lactamase positive bacteria. These organisms produce enzymes that can break down beta-lactam antibiotics, rendering them ineffective. This resistance poses a significant challenge in healthcare, especially as antibiotic resistance continues to rise.
In this article, you’ll discover what it means for a bacterium to be beta lactamase positive, along with real-world examples of these resistant strains. We’ll explore how they affect treatment options and public health efforts. You’ll gain insights into the implications for both patients and medical professionals, making it clear why understanding this topic is crucial in today’s fight against infections. Are you ready to dive deeper into the world of antibiotic resistance?
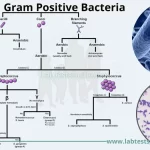
Overview of Beta Lactamase Positive Bacteria
Beta lactamase positive bacteria produce enzymes that can break down beta-lactam antibiotics. This resistance poses a significant challenge in treating bacterial infections. Some common examples include:
- Escherichia coli: Many strains show resistance due to extended-spectrum beta-lactamases (ESBLs), complicating treatment options.
- Klebsiella pneumoniae: Known for its ability to produce carbapenemases, making it resistant to multiple antibiotic classes.
- Staphylococcus aureus: Methicillin-resistant Staphylococcus aureus (MRSA) produces beta-lactamase enzymes, limiting the effectiveness of commonly used penicillins.
It’s essential to recognize these bacteria in clinical settings. They can lead to severe infections and increased healthcare costs. Do you realize how much impact antibiotic resistance has on patient outcomes? Understanding these examples helps guide appropriate treatment strategies and infection control measures.
Mechanism of Beta Lactamase Production
Beta-lactamase enzymes break down beta-lactam antibiotics, making them ineffective. Understanding the mechanisms behind their production is essential for addressing antibiotic resistance.
Genetic Factors
Genes play a crucial role in the production of beta-lactamases. Various bacteria harbor beta-lactamase genes that enable them to produce these enzymes. For instance:
- TEM and SHV genes: Commonly found in Escherichia coli and Klebsiella pneumoniae, these genes contribute to extended-spectrum beta-lactamases (ESBLs).
- CTX-M genes: Associated with increased resistance, especially in community-acquired infections.
These genetic factors can be transferred between bacteria through horizontal gene transfer, increasing resistance.
Environmental Influences
Environmental factors significantly impact beta-lactamase production. Conditions such as:
- Antibiotic exposure: Frequent use of antibiotics promotes selection for resistant strains.
- Hospital settings: High antibiotic consumption in healthcare facilities fosters environments where resistant bacteria thrive.
Such influences lead to higher prevalence rates of beta-lactamase positive strains, complicating treatment options and infection control measures.
Types of Beta Lactamases
Beta-lactamases are categorized into several classes based on their molecular structure and enzymatic activity. Understanding these types helps in identifying the mechanisms behind antibiotic resistance.
Class A Beta Lactamases
Class A beta-lactamases primarily target penicillins and cephalosporins. Examples include TEM-1 and SHV-1, which are found in various Enterobacteriaceae. These enzymes often hydrolyze extended-spectrum cephalosporins, complicating treatment options. The prevalence of Class A enzymes makes them a significant concern in hospital settings where infections like those caused by Klebsiella pneumoniae are common.
Class B Beta Lactamases
Class B beta-lactamases, also known as metallo-beta-lactamases (MBLs), require zinc ions for their activity. They can hydrolyze a broad range of beta-lactams, including carbapenems, making them particularly dangerous. Notable examples include IMP and VIM types, often associated with multi-drug resistant strains like Pseudomonas aeruginosa. Their presence indicates severe treatment challenges in infections that typically respond to standard antibiotics.
Class C Beta Lactamases
Class C beta-lactamases mainly affect cephalosporins and are commonly found in species such as Enterobacter and Citrobacter. An example is AmpC, which can be overexpressed under certain conditions, leading to increased resistance levels. Infections caused by bacteria producing these enzymes can result in higher mortality rates due to limited effective treatments available.
Understanding these classes aids healthcare professionals in choosing appropriate therapies against resistant bacterial infections effectively.
Clinical Implications of Beta Lactamase Positive Infections
Beta lactamase positive infections present significant challenges in clinical settings. These bacteria produce enzymes that degrade beta-lactam antibiotics, undermining treatment effectiveness and complicating patient care.
Treatment Challenges
Infections caused by beta lactamase positive bacteria often lead to limited treatment options. Conventional antibiotics may prove ineffective, requiring healthcare providers to consider alternatives such as:
- Carbapenems: Despite their broad spectrum, certain strains exhibit resistance.
- Aminoglycosides: May be utilized but come with toxicity risks.
- Polymyxins: Effective against resistant Gram-negative bacteria, yet can cause nephrotoxicity.
Moreover, combination therapy might become necessary to enhance efficacy. Yet, the decision-making process remains complex due to potential side effects and the risk of further resistance development.
Resistance Patterns
The patterns of antibiotic resistance among beta lactamase positive strains are concerning. For instance:
- Escherichia coli: Often exhibits CTX-M type beta-lactamases, leading to community-acquired urinary tract infections resistant to common treatments.
- Klebsiella pneumoniae: Frequently harbors KPC-type beta-lactamases, associated with outbreaks in healthcare facilities.
- Staphylococcus aureus: Methicillin-resistant Staphylococcus aureus (MRSA) strains can also produce beta-lactamases, complicating management strategies.
You might wonder how these resistance patterns impact public health. Indeed, they contribute significantly to increased morbidity and mortality rates. Addressing infection control measures becomes crucial for mitigating these risks effectively.