Are you curious about how ACO examples can transform healthcare delivery? As the healthcare landscape evolves, understanding these innovative models becomes crucial. Accountable Care Organizations (ACOs) aim to provide high-quality care while reducing costs, making them a hot topic in today’s discussions.
In this article, you’ll explore various ACO examples that showcase effective strategies and real-world applications. From successful collaborations between hospitals and primary care providers to community-based initiatives that prioritize patient outcomes, these cases illustrate the potential of ACOs. Get ready to dive into inspiring stories that highlight how organizations are reshaping care for millions. Are you ready to discover what makes these ACO examples stand out?
Overview of ACO Examples
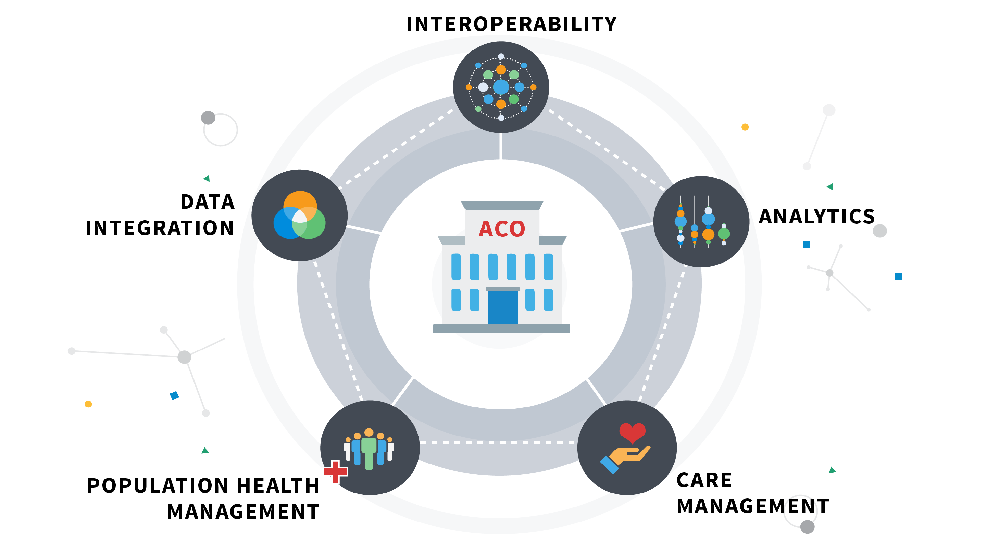
Accountable Care Organizations (ACOs) represent innovative models in healthcare, focusing on improving patient care while managing costs. Various examples highlight how these organizations operate effectively in diverse settings.
Definition of ACO
An ACO is a group of healthcare providers that come together to deliver coordinated care to patients. These organizations aim for high-quality services by working collaboratively across different specialties and facilities. They share responsibility for patient outcomes, which promotes accountability among providers.
Importance of ACO in Healthcare
Understanding the significance of ACOs in healthcare is crucial. They emphasize preventive care and chronic disease management, leading to better health outcomes and lower expenses. Here are some key reasons why ACOs matter:
- Improved Quality: ACOs focus on evidence-based practices that enhance patient satisfaction.
- Cost Efficiency: By reducing unnecessary tests and procedures, they help lower overall healthcare costs.
- Patient-Centered Care: Emphasizing personalized treatment plans fosters better relationships between patients and providers.
Each example demonstrates how collaboration within an ACO can lead to substantial improvements in both quality and efficiency.
Successful ACO Examples
Understanding successful Accountable Care Organizations (ACOs) provides insight into effective healthcare models. Here are two prominent examples highlighting how different structures achieve improved patient care and cost efficiency.
Example 1: Integrated Health System
Integrated health systems exemplify collaboration among various healthcare providers. These organizations include hospitals, outpatient facilities, and specialty practices that work together seamlessly. They focus on coordinated care to enhance patient outcomes while managing costs effectively.
Key features of integrated health systems include:
- Shared electronic health records for real-time data access.
- Standardized treatment protocols that ensure consistency in care.
- Comprehensive wellness programs aimed at prevention and chronic disease management.
By fostering teamwork among providers, integrated health systems significantly reduce hospital readmission rates and improve overall patient satisfaction.
Example 2: Physician-Led Organization
Physician-led organizations prioritize physician engagement in decision-making processes. In these ACOs, doctors lead initiatives focused on enhancing clinical quality and reducing unnecessary expenditures. This structure empowers physicians to implement changes directly impacting patient care.
Essential components of physician-led organizations encompass:
- Direct involvement in policy-making, allowing tailored approaches to local needs.
- Data analytics tools that help track patient outcomes efficiently.
- Incentive programs rewarding high-quality performance over volume of services provided.
Such leadership often results in more personalized care experiences for patients, contributing to better health outcomes across diverse communities.
Challenges Faced by ACOs
Accountable Care Organizations (ACOs) encounter several challenges that can impede their effectiveness. Understanding these obstacles helps in developing strategies to navigate them.
Common Obstacles
- Data Sharing Difficulties: ACOs often struggle with integrating data from multiple sources. Inconsistent electronic health record systems can lead to gaps in patient information.
- Financial Risk Management: Managing financial risk proves challenging, especially when it comes to shared savings models. Fluctuating healthcare costs can impact an ACO’s profitability.
- Patient Engagement Issues: Engaging patients in their care remains a significant hurdle. Many patients may lack awareness or motivation to participate actively in their health management.
- Regulatory Compliance: Navigating complex regulations is demanding for ACOs. Adhering to evolving policies requires constant monitoring and adjustments.
- Provider Alignment: Achieving alignment among diverse providers poses another challenge. Different priorities and incentives can create conflicts within the organization.
- Enhanced Data Systems: Implementing advanced data-sharing platforms helps streamline communication between providers, ensuring all stakeholders have access to real-time patient information.
- Risk Assessment Tools: Utilizing sophisticated risk assessment tools enables better financial forecasting and management of shared savings arrangements, enhancing overall stability.
- Patient Education Programs: Developing targeted education programs fosters greater patient understanding regarding their roles in care, boosting engagement levels significantly.
- Compliance Training Sessions: Regular compliance training ensures that all team members stay informed about regulatory updates, promoting adherence across the organization.
- Collaborative Culture Initiatives: Fostering a culture of collaboration encourages alignment among providers by highlighting shared goals and collective success metrics, ultimately driving improved outcomes for patients and organizations alike.
By addressing these challenges head-on with effective strategies, ACOs can enhance their operations and better serve patient populations while achieving desired health outcomes efficiently.
Future of ACO Models
The future of Accountable Care Organizations (ACOs) holds significant potential for enhancing healthcare delivery. As the landscape evolves, innovations and predicted trends will shape how ACOs operate and impact patient care.
Innovations in ACOs
Innovations are transforming ACO models to improve efficiency and patient outcomes. For instance, data analytics tools enable real-time tracking of patient health metrics, allowing providers to intervene earlier. Additionally, telehealth services have become crucial, expanding access to care while reducing costs.
Other noteworthy innovations include:
- Integrated health technologies that streamline communication among providers.
- Patient engagement platforms that encourage active participation in care decisions.
- Artificial intelligence systems that predict patient needs based on historical data.
These advancements not only enhance coordination but also promote a proactive approach to healthcare.
Predicted Trends
Several trends are expected to influence the future of ACOs significantly. First, there’s a shift towards value-based care models emphasizing quality over quantity. As reimbursement models evolve, focusing on improving health outcomes gains priority.
Moreover, expect an increase in collaboration between various stakeholders:
- Hospitals partnering with local organizations for community health initiatives.
- Payors incentivizing ACOs for achieving specific performance metrics.
Also, enhanced regulatory frameworks may emerge to support innovation within ACO structures while ensuring accountability and transparency. These trends indicate a dynamic future where ACOs play an even more vital role in delivering high-quality healthcare efficiently.